An innovative monopegylated interferon that provides long-term chronic dosing1
1 subcutaneous dose every 2 weeks
Hematologic stability defined
<45%
<10 x 109/L
<400 x 109/L
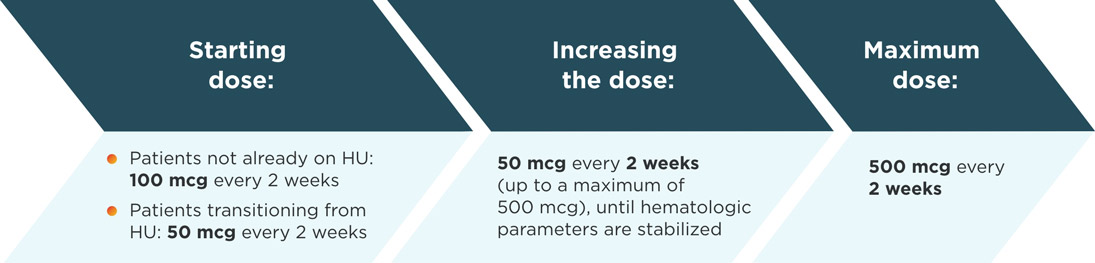
Dose titration1
Patients not already on HU
Increase the dose by 50 mcg every 2 weeks (up to a maximum of 500 mcg), until hematologic parameters are stabilized.
Patients transitioning from HU
Gradually taper off HU by reducing the total biweekly dose by 20% to 40% every 2 weeks during Weeks 3-12.
Increase the dose of BESREMi by 50 mcg every 2 weeks (up to a maximum of 500 mcg), until hematologic parameters are stabilized.
Discontinue HU by Week 13.
Maintain the 2-week dosing interval of BESREMi at which hematologic stability is achieved for at least 1 year. After that time, the dosing interval may be expanded to 1 dose every 4 weeks.1
- All eligible patients in the PEGINVERA study (n=28) switched to 1 dose every 4 weeks as early as 1 year after starting BESREMi
- The mean dose of BESREMi was 237 mcg (±110) during the treatment period
Dose modifications1
- Monitor complete blood counts (CBC) every 2 weeks during the titration phase and dose modification phase, and every 3-6 months during the maintenance phase (after the patient’s optimal dose is established). Monitor CBC more frequently if clinically indicated
- Phlebotomy as rescue treatment to normalize blood hyperviscosity may be necessary
- If dose interruption occurs, resume dosing at previously attained levels
- If drug-related toxicities arise, reduce the dose to the next lower level or interrupt in accordance with the table below
- If there is insufficient efficacy at the decreased dose following dose modification, a dose increase attempt to the next higher dose level should be considered after recovery to grade 1 toxicity
| ADVERSE REACTION* | SEVERITY | DOSAGE MODIFICATION |
|---|---|---|
| Liver enzyme elevation with concomitant bilirubin elevation, or other evidence of hepatic decompensation | Any increase above baseline | Interrupt treatment until recovery, restart at dose 50 mcg lower than the interrupted dose. If the interrupted dose is 50 mcg, refrain from treatment until recovery. Consider permanent discontinuation if toxicity persists after four dose-modifications. |
| Liver enzyme elevation | >5 x the upper limit of normal (ULN) but ≤20 x ULN | Decrease dose by 50 mcg; if toxicity does not improve, continue decreasing at biweekly intervals until alanine aminotransferase (ALT) and aspartate aminotransferase (AST) recover <3 x ULN if baseline was normal; 3 x baseline if baseline was abnormal, and gamma-glutamyltransferase (GGT) recovers to <2.5 x ULN if baseline was normal; 2.5 x baseline if baseline was abnormal. If the interrupted dose is 50 mcg, refrain from treatment until recovery. |
| >20 x ULN | Interrupt treatment until ALT and AST recover to <3 x ULN if baseline was normal; 1.5 x baseline if baseline was abnormal, and gamma-glutamyltransferase (GGT) recovers to <2.5 x ULN if baseline was normal; 2 x baseline if baseline was abnormal. Consider permanent discontinuation if toxicity persists after four dose-modifications. | |
| Cytopenia | Anemia: hemoglobin (Hgb) <8 g/dL Thrombocytopenia: platelet count <50,000/mm3 but ≥25,000/mm3 Leukopenia: white blood cell count (WBC) <2,000/mm3 but ≥1,000/mm3 | Decrease dose by 50 mcg; if toxicity does not improve, continue decreasing at biweekly intervals until recovery of Hgb >10.0 g/dL, platelets >75,000/mm3, and WBC >3,000/mm3. If the interrupted dose is 50 mcg, refrain from treatment until recovery. |
| Anemia: hemoglobin levels are life threatening, or urgent intervention needed Thrombocytopenia: platelet count <25,000/mm3 Leukopenia: WBC <1,000/mm3 | Interrupt treatment until recovery of Hgb >10.0 g/dL, platelets >75,000/mm3, and WBC >3,000/mm3. Consider permanent discontinuation if toxicity persists after four dose-modifications. | |
| Depression | Mild, without suicidal ideation | Consider psychiatric consultation if persistent (>8 weeks). |
| Moderate, without suicidal ideation | Consider dose reduction and psychiatric consultation. | |
| Severe, or any severity with suicidal ideation | Discontinue therapy, recommend psychiatric consultation. |
*National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 3.0.
INDICATION
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
- Existence of, or history of severe psychiatric disorders, particularly severe depression, suicidal ideation, or suicide attempt
- Hypersensitivity to interferons including interferon alfa-2b or any of the inactive ingredients of BESREMi.
- Moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment
- History or presence of active serious or untreated autoimmune disease
- Immunosuppressed transplant recipients
WARNINGS AND PRECAUTIONS
Depression and Suicide: Life-threatening or fatal neuropsychiatric reactions have occurred in patients receiving interferon alfa-2b products, including BESREMi. These reactions may occur in patients with and without previous psychiatric illness.
Other central nervous system effects, including suicidal ideation, attempted suicide, aggression, bipolar disorder, mania and confusion have been observed with other interferon alfa products.
Closely monitor patients for any symptoms of psychiatric disorders and consider psychiatric consultation and treatment if such symptoms emerge. If psychiatric symptoms worsen, it is recommended to discontinue BESREMi therapy.- Endocrine Toxicity: These toxicities may include worsening hypothyroidism and hyperthyroidism. Do not use BESREMi in patients with active serious or untreated endocrine disorders associated with autoimmune disease. Evaluate thyroid function in patients who develop symptoms suggestive of thyroid disease during BESREMi therapy. Discontinue BESREMi in patients who develop endocrine disorders that cannot be adequately managed during treatment with BESREMi.
- Cardiovascular Toxicity: Toxicities may include cardiomyopathy, myocardial infarction, atrial fibrillation and coronary artery ischemia. Patients with a history of cardiovascular disorders should be closely monitored for cardiovascular toxicity during BESREMi therapy. Avoid use of BESREMi in patients with severe or unstable cardiovascular disease, (e.g., uncontrolled hypertension, congestive heart failure (≥ NYHA class 2), serious cardiac arrhythmia, significant coronary artery stenosis, unstable angina) or recent stroke or myocardial infarction.
- Decreased Peripheral Blood Counts: These toxicities may include thrombocytopenia (increasing the risk of bleeding), anemia, and leukopenia (increasing the risk of infection). Monitor complete blood counts at baseline, during titration and every 3-6 months during the maintenance phase. Monitor patients for signs and symptoms of infection or bleeding.
- Hypersensitivity Reactions: Toxicities may include serious, acute hypersensitivity reactions (e.g., urticaria, angioedema, bronchoconstriction, anaphylaxis). If such reactions occur, discontinue BESREMi and institute appropriate medical therapy immediately. Transient rashes may not necessitate interruption of treatment.
- Pancreatitis: Pancreatitis has occurred in 2.2% of patients receiving BESREMi. Symptoms may include nausea, vomiting, upper abdominal pain, bloating, and fever. Patients may experience elevated lipase, amylase, white blood cell count, or altered renal/hepatic function. Interrupt BESREMi treatment in patients with possible pancreatitis and evaluate promptly. Consider discontinuation of BESREMi in patients with confirmed pancreatitis.
- Colitis: Fatal and serious ulcerative or hemorrhagic/ischemic colitis have occurred in patients receiving interferon alfa products, some cases starting as early as 12 weeks after start of treatment. Symptoms may include abdominal pain, bloody diarrhea, and fever. Discontinue BESREMi in patients who develop these signs or symptoms. Colitis may resolve within 1 to 3 weeks of stopping treatment.
- Pulmonary Toxicity: Pulmonary toxicity may manifest as dyspnea, pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension, and sarcoidosis. Some events have resulted in respiratory failure or death. Discontinue BESREMi in patients who develop pulmonary infiltrates or pulmonary function impairment.
- Ophthalmologic Toxicity: These toxicities may include severe eye disorders such as retinopathy, retinal hemorrhage, retinal exudates, retinal detachment and retinal artery or vein occlusion which may result in blindness. During BESREMi therapy, 23% of patients were identified with an eye disorder. Eyes disorders ≥5% included cataract (6%) and dry eye (5%). Advise patients to have eye examinations before and during BESREMi therapy, specifically in those patients with a retinopathy-associated disease such as diabetes mellitus or hypertension. Evaluate eye symptoms promptly. Discontinue BESREMi in patients who develop new or worsening eye disorders.
- Hyperlipidemia: Elevated triglycerides may result in pancreatitis. Monitor serum triglycerides before BESREMi treatment and intermittently during therapy and manage when elevated. Consider discontinuation of BESREMi in patients with persistently, markedly elevated triglycerides.
- Hepatotoxicity: These toxicities may include increases in serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT) and bilirubin. Liver enzyme elevations have also been reported in patients after long-term BESREMi therapy. Monitor liver enzymes and hepatic function at baseline and during BESREMi treatment. Discontinue BESREMi in patients who develop evidence of hepatic decompensation (characterized by jaundice, ascites, hepatic encephalopathy, hepatorenal syndrome or variceal hemorrhage) during treatment
- Renal Toxicity: Monitor serum creatinine at baseline and during therapy. Avoid use of BESREMi in patients with eGFR <30 mL/min. Discontinue BESREMi if severe renal impairment develops during treatment.
- Dental and Periodontal Toxicity: These toxicities may include dental and periodontal disorders, which may lead to loss of teeth. In addition, dry mouth could have a damaging effect on teeth and mucous membranes of the mouth during long-term treatment with BESREMi. Patients should have good oral hygiene and regular dental examinations.
- Dermatologic Toxicity: These toxicities have included skin rash, pruritus, alopecia, erythema, psoriasis, xeroderma, dermatitis acneiform, hyperkeratosis, and hyperhidrosis. Consider discontinuation of BESREMi if clinically significant dermatologic toxicity occurs.
- Driving and Operating Machinery: BESREMi may impact the ability to drive and use machinery. Patients should not drive or use heavy machinery until they know how BESREMi affects their abilities. Patients who experience dizziness, somnolence or hallucination during BESREMi therapy should avoid driving or using machinery.
- Embryo-Fetal Toxicity: Based on the mechanism of action, BESREMi can cause fetal harm when administered to a pregnant woman. Pregnancy testing is recommended in females of reproductive potential prior to treatment with BESREMi. Advise females of reproductive potential to use an effective method of contraception during treatment with BESREMi and for at least 8 weeks after the final dose.
ADVERSE REACTIONS
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Pregnancy: Based on mechanism of action and the role of interferon alfa in pregnancy and fetal development, BESREMi may cause fetal harm and should be assumed to have abortifacient potential when administered to a pregnant woman. There are adverse effects on maternal and fetal outcomes associated with polycythemia vera in pregnancy. Advise pregnant women of the potential risk to a fetus.
- Lactation: There are no data on the presence of BESREMi in human or animal milk, the effects on the breastfed child, or the effects on milk production. Because of the potential for serious adverse reactions in breastfed children from BESREMi, advise women not to breastfeed during treatment and for 8 weeks after the final dose.
- Females of Reproductive Potential: BESREMi may cause embryo-fetal harm when administered to a pregnant woman. Pregnancy testing prior to BESREMi treatment is recommended for females of reproductive potential. Advise female patients of reproductive potential to use effective contraception during treatment with BESREMi and for at least 8 weeks after the final dose.
- Pediatric Use: Safety and effectiveness in pediatric patients have not been established.
- Geriatric Use: In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other therapy.